Table of Contents
What is cystectomy and why is it done?
Cystectomy (sis-TEK-toh-mee) is a major surgery that is used to treat bladder cancer. There are two types of cystectomies that you need to know about:
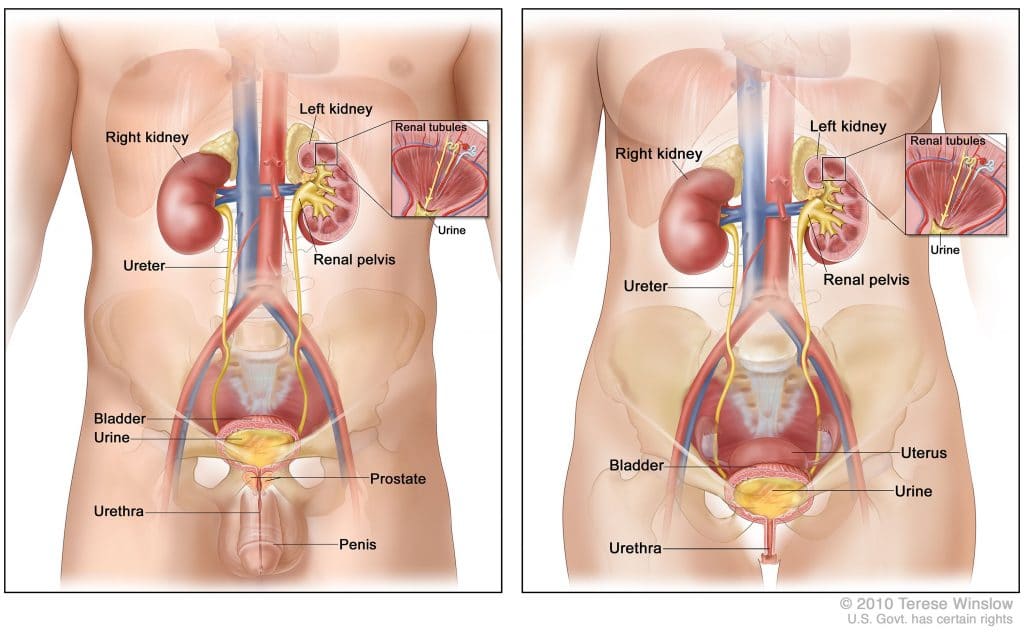
- Radical cystectomy: Surgery to remove the bladder and any lymph nodes and nearby organs that contain cancer. This surgery may be done when the bladder cancer invades the muscle wall, or when superficial cancer involves a large part of the bladder.
In men, the nearby organs that are removed are the prostate and the seminal vesicles. In women, the uterus, the ovaries, and part of the vagina are removed.
Sometimes, when the cancer has spread outside the bladder and cannot be completely removed, surgery to remove only the bladder may be done to reduce urinary symptoms caused by the cancer.
When the bladder must be removed, the surgeon creates another way for urine to leave the body (this is called a “urinary diversion”). - Partial cystectomy: Surgery to remove part of the bladder. This surgery may be done for patients who have a low-grade tumor that has invaded the wall of the bladder but is limited to one area of the bladder. Because only a part of the bladder is removed, patients are able to urinate normally after recovering from this surgery. This is also called segmental cystectomy.
Sometimes cystectomy is done for other reasons like:
- failure of or recurrence after a bladder-sparing approach (chemoradiation) or the occurrence of major side-effects
- symptoms like bleeding or pain in patients with non-curable disease
Preparing for cystectomy
You will likely undergo an evaluation by a multidisciplinary team (for example, urologist, surgeon, anaesthesiologist, primary care, cardiologist) before this surgery.
Factors like your biological age (your body’s performance as it ages, measured as performance status or life expectancy) and other diseases that you have (diabetes, heart disease, high blood pressure) are also important. Patients older than 80 years of age have more problems recovering from such an operation. Physicians use special indexed scores to assess the risk of patients undergoing this stressful operation.
Prior abdominal surgery or radiotherapy makes surgery more difficult but is rarely a reason not to have surgery. Being overweight does not influence survival after surgery but does influence the risk of complications from wound healing.
Removal of the urinary bladder includes removal of the bladder, the endings of the ureters and the pelvic lymph nodes. Depending on factors like tumour location and type of urinary diversion part of the adjacent gender-specific organs (the prostate and seminal vesicles in men; the entire urethra, adjacent vagina, and uterus in women) are removed. Men should be aware that prostate cancer is sometimes found in removed prostates but generally does not affect long-term survival or treatment.
How is the bladder removed?
Before the surgery
Before surgery, your doctor will inform you in detail how to prepare for anaesthesia. If you are taking any medications, discuss them with your doctor. You may need to stop taking medications for several days before surgery.
You will typically be admitted to the hospital 1 day prior to the operation. A physician or nurse will talk you through the operation and explain what happens before and especially after the surgery.
Part of your intestines will be used to create the urinary diversion. Your doctor will advise you in detail about how to prepare for the procedure.
During the surgery
Removal of the urinary bladder is performed through an incision in the abdomen (open) with the patient under general anaesthesia (combination of intravenous drugs and inhaled gasses; you are ‘asleep’). The bladder, the ends of the ureters close to the bladder, the pelvic lymph nodes, and (part of) adjacent gender-specific organs are removed. Now another way to store and empty urine must be created (urinary diversion).
This surgery can be done as an open or a laparoscopic or robotic-assisted procedure at centres that treat a lot of patients and have experienced and specialized surgeons. This surgery typically takes 3 to 6 hours, not including recovery time.
After the SURGERY
For the first few days you will be closely monitored. To prevent blood clots after the operation, you will likely receive medication for up to 4 weeks in the form of injections or pills. Your doctor will inform you in detail about the post-operative routine.
During hospitalisation, you will learn how to manage the urostomy or neobladder. Once you have learned how to use and empty the urostomy or internal urine pouch, a date for your discharge will be set.
What to expect back home
You may have some discomfort or pain for a few weeks after surgery. Ask your doctor or nurse about ways to manage pain and be comfortable as you heal. If you have any side effects/complications or feel any symptoms that you are unable to explain/are unexpected, contact your surgery team immediately.
Physical activity after the procedure
Your physical activities will be limited after surgery, but it is important to stay active. The exact details of exercise and any limitations will be provided by your surgery team. In general, light activity like walking can help recovery. Avoid lifting more than 5 kg (about the weight of a house cat). Ask your doctor or nurse about when you can resume driving and bathing. Your strength and energy will come back gradually.
Chemotherapy before removal of the bladder
Chemotherapy is administered before bladder removal (also called neoadjuvant chemotherapy) to potentially shrink the tumour and kill cells that have already entered the blood or lymph nodes.
Chemotherapy before the operation may be recommended for patients with muscle-invasive disease (at least stage 2 disease). It is also necessary if tumors are large (>3 cm) or if signs indicate that cancer has spread to the lymph nodes (metastatic disease) and the goal is treatment of the disease. The decision to administer chemotherapy is made by a multidisciplinary team (including an oncologist, a urologist, and sometimes, a radiation oncologist).
Adequate kidney function is necessary. Potential side-effects are usually monitored and managed by an oncologist. A typical chemotherapy regimen used for bladder cancer is cisplatin and gemcitabine – you can read about it in detail here.
A good response to chemotherapy improves survival but does not change the need for surgery. Although neoadjuvant chemotherapy is currently advised, physicians are unable to identify who will definitely benefit from chemotherapy before removal of the bladder.
Chemotherapy after removal of the bladder
If a tumor is large (>3 cm), or could not be fully removed, or if cancer has spread to the lymph nodes (determined by the pathologist), chemotherapy after removal of the bladder is an option. Cancer that has spread to the lymph nodes indicates systemic disease and may need systemic treatment (with chemotherapy or immunotherapy) in certain cases.
Impact on life
Sex life after radical cystectomy
Ask your doctor or stoma nurse/specialised nurse when it’s safe to resume sexual activities. You should wait at least six weeks before sexual intercourse to allow proper healing to take place.
Your sex life might be affected after having surgery for bladder cancer. This depends on the type of surgery you have.
Your body may look different after the surgery, which may take time to get used to. For men, the penis may appear slightly shorter than before the surgery. For both men and women, having a stoma can also affect the way you feel about yourself and how you feel about having sex. Take your time to recover. You will feel when you are ready to start sexual intercourse again. In the meanwhile spend time with your partner, share interest, enjoy cuddling and do not stop talking with each other.
Impact on Men
Bladder removal for men typically includes removing the prostate. This is done to prevent bladder cancer coming back in the prostate later.
Without a prostate, you will not be able to produce semen fluid. You can still have an orgasm, but your orgasms will be dry (without semen). Sperm cells can still be produced in the testicles but you cannot make a partner pregnant by sexual intercourse. Talk with your doctor before surgery if you have questions about fertility.
Your ability to have an erection may be affected. Cystectomy can damage the nerves that control erection. Talk with your doctor if you have questions about sex or fertility.
If the nerves are not damaged, you might still need assistance to get an erection after surgery. Ask your doctor or nurse what techniques might work for you. Several options exist and can be used alone or together:
Impact on Women
Bladder removal for women typically includes removing the internal sexual organs, including the uterus, ovaries and the part of the vagina that is next to the bladder and urethra. This is not necessary in every case, but is typically done to make sure all the cancer is removed. In some cases, it is possible to preserve the internal sexual organs, depending on the location of the tumour in the bladder. The labia and clitoris are not removed, and most of the vagina will usually be left, so most women will still be able to have an orgasm and intercourse.
It may take time to get used to how this looks and feels. Sex may feel different than it did before surgery. You might have less sexual desire. You might need to use a gel to help with lubrication. Treatment is available if intercourse is painful (dyspareunia). Talk with your partner and your doctor or nurse about these problems.
Last updated- 6/3/21A