Table of Contents
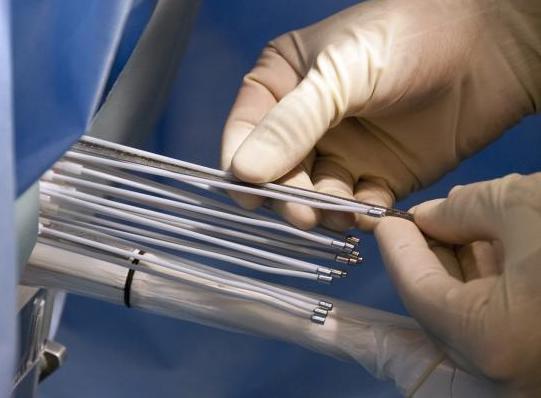
Brachytherapy is a procedure to implant radioactive seeds (pellets) into the prostate gland to kill prostate cancer cells. The seeds may give off high or low amounts of radiation.
Types of brachytherapy:
- Low-dose rate brachytherapy is the most common type of treatment. The seeds stay inside your prostate and put out a small amount of radiation for several months. You go about your normal routine with the seeds in place.
- High-dose rate brachytherapy lasts about 30 minutes. Your doctor inserts the radioactive material into the prostate. The doctor may use a computerized robot to do this. The radioactive material is removed right away after treatment. This method often requires 2 treatments spaced 1 week apart.
Why is brachytherapy given?
Brachytherapy is often used for men with prostate cancer that is found early and is slow-growing. Brachytherapy has fewer complications and side effects than standard radiation therapy. You will also need fewer visits with the health care provider.
How is brachytherapy given?
Brachytherapy takes 30 minutes or more, depending on the type of therapy you have. Before the procedure, you will be given medicine so that you do not feel pain. You may receive:
- A sedative to make you drowsy and numbing medicine on your perineum. This is the area between the anus and scrotum.
- Anesthesia: With spinal anesthesia, you will be drowsy but awake, and numb below the waist. With general anesthesia, you will be asleep and pain free.
After you receive anesthesia:
- The doctor places an ultrasound probe into your rectum to view the area. The probe is like a camera connected to a video monitor in the room. A catheter (tube) may be placed in your bladder to drain urine.
- The doctor uses ultrasound or a CT scan to plan and then place the seeds that deliver radiation into your prostate. The seeds are placed with needles or special applicators through your perineum.
- Placing the seeds may hurt a little (if you are awake).
What risks can I expect from brachytherapy?
Risks of any anesthesia are:
- Allergic reactions to medicines
- Breathing problems
Risks of any surgery are:
- Bleeding
- Infection
Risks of this procedure are:
- Impotence
- Difficulty emptying your bladder, and the need to use a catheter
- Rectal urgency, or the feeling that you need to have a bowel movement right away
- Skin irritation in your rectum or bleeding from your rectum
- Other urinary problems
- Ulcers (sores) or a fistula (abnormal passage) in the rectum, scarring and narrowing of the urethra (all of these are rare)
Ask your medical team about additional risks specific to your situation.
Preparing for the procedure
Tell your provider what medicines you are taking. These include medicines, supplements, or herbs you bought without a prescription.
Before this procedure:
- You may need to have ultrasounds, x-rays, or CT scans to prepare for the procedure.
- Several days before the procedure, you may be told to stop taking medicines that make it hard for your blood to clot. These medicines include aspirin, ibuprofen (Advil), clopidogrel (Plavix), and warfarin (Coumadin).
- Ask which medicines you should still take on the day of the surgery.
- If you smoke, try to stop. Your provider can help.
On the day of the procedure:
- You will likely be asked not to drink or eat anything for several hours before the procedure.
- Take the medicines you’ve been told to take with a small sip of water.
- You will be told when to arrive at the hospital. Be sure to arrive on time.
After the procedure and safety instructions for family
You may be sleepy and have mild pain and tenderness after the procedure. After an outpatient procedure, you can go home as soon as the anesthesia wears off. In rare cases, you will need to spend 1 to 2 days in the hospital. If you stay in the hospital, your visitors will need to follow special radiation safety precautions.
Some blood in your urine or semen can be expected for a few days. You may need to use a urinary catheter for 1 or 2 days if you have a lot of blood in your urine. Your health care provider will show you how to use it. You may also feel the urge to urinate more often. Your perineum may be tender and bruised. You can use ice packs and take pain medicine to ease discomfort.
If you have a permanent implant, your provider may tell you to limit the amount of time you spend around children and women who are pregnant. After a few weeks to months, the radiation is gone and will not cause any harm. Because of this, there is no need to take out the seeds.
Activity
- Take it easy when you return home. Mix light activity with periods of rest to help speed your recovery.
- Avoid heavy activity (such as housework, yard work, and lifting children) for at least 1 week. You should be able to return to your normal activities after that. You can resume sexual activity when you feel comfortable.
- If you have a permanent implant, ask your provider if you need to limit your activities. You will probably need to avoid sexual activity for about 2 weeks, and then use a condom for several weeks after that.
- Try not to let children sit on your lap in the first few months after treatment because of possible radiation from the area.
Self-care
- Apply ice packs to the area for 20 minutes at a time to reduce pain and swelling. Wrap ice in a cloth or towel. DO NOT put the ice directly on your skin.
- Take your pain medicine as your doctor told you to.
- You may go back to your regular diet when you get home. Drink 8 to 10 glasses of water or unsweetened juice a day and choose healthy foods. Avoid alcohol for the first week.
- You may shower and gently wash the perineum with a washcloth. Pat dry the tender areas. DO NOT soak in a bath tub, hot tub, or go swimming for 1 week.
Follow-up
You may need to have follow up visits with your provider for more treatment or imaging tests. Make sure to follow all post-procedure instructions given by your medical team.
When to Call the Doctor
Call your health care provider if you have:
- Fever greater than 101°F (38.3°C) and chills
- Severe pain in your rectum when you urinate or at other times
- Blood or blood clots in your urine
- Bleeding from your rectum
- Problems having a bowel movement or passing urine
- Shortness of breath
- Severe discomfort in the treatment area that does not go away with pain medicine
- Drainage from the place the catheter was inserted
- Chest pain
- Abdominal (belly) discomfort
- Severe nausea or vomiting
- Any new or unusual symptoms
Outlook (Prognosis)
Most men with small, slow-growing prostate cancer remain cancer-free or their cancer is in good control for many years after this treatment. Urinary and rectal symptoms may last for months or years.
Alternative Names
Implant therapy – prostate cancer; Radioactive seed placement; Internal radiation therapy – prostate; High dose radiation (HDR)