Table of Contents
Colon Anatomy
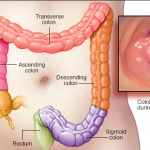
The colon or the large intestine is an essential organ of the digestive system. The colon is the distal part of the GI tract which averages 150 cm in length.
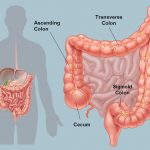
After going through the stomach, the food enters the small intestine, where the body absorbs most of its nutrients. The remaining waste products then move into the colon, where the body removes as much fluid and remaining nutrients as possible. The colon then makes this waste into the stool and eliminates it.
The colon absorbs water and electrolytes from the digested food to form faeces.
Anatomically, the colon has three sections, ascending, transverse, descending, and sigmoid. These sections include an arch, which encircles the small intestine.
Colon cancer
Colon cancer begins in the large intestine. It primarily affects adults, though it may happen at any age. It starts as small, noncancerous (benign) clumps of cells called polyps inside the colon. Some of these polyps can become malignant. Hence, regular screening tests are necessary to prevent colon cancer by identifying and removing polyps before turning malignant.
Signs and symptoms
- A change in bowel habits (diarrhea, constipation, or narrowing of the stool)
- A feeling of having frequent bowel movement
- Rectal bleeding
- Blood in the stool making the stool look dark brown or black
- Cramps or abdominal pain
- Weakness and fatigue
- Unintended weight loss
Colon surgery may be an option if:
- Colonoscopy could not remove all the polyps. Surgery is needed to remove the polyp because it may contain cancer cells that could spread over time.
- A polyp has invasive cancer cells. The polyp tissue is checked for cancer. The presence of cancer cells ensures surgery because cancer may have spread beyond the polyp.
- Stage I, II, or III colon cancer is detected. It doesn’t spread to distant parts of the body to remove entire cancer with surgery.
- Stage IV (advanced) colon cancer is detected, spreading to parts of the liver or lungs that can be eliminated with surgery.
- Advanced cancer is obstructing the colon or causing other significant problems. In these cases, surgery may be used to fix the problem and ease symptoms.
Types of colon cancer surgeries
Colon surgery is the first line of treatment against colon cancer. It is an essential component of colon cancer treatment that involves the removal of cancer with an operation. It may be performed alone or combined with other therapies, such as chemotherapy, immunotherapy, hormone therapy, targeted therapy, and radiation therapy.
Surgery is the primary treatment for early-stage colon cancers. It depends on the cancer stage and tumor location. The surgery needs to be done on a clean and empty colon. Before surgery, a special diet and laxative drinks or enemas are suggested to get the stool out of the colon.
If colon cancer is minimal, your doctor may recommend a minimally invasive approach to surgery, such as:
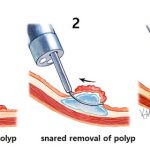
Polypectomy
A polypectomy removes polyps or abnormal collection of tissue from the inside of the colon. The procedure is non-invasive and is performed at the same time as a colonoscopy. Polyps are often associated with no symptoms. However, large polyps may cause rectal bleeding, abdominal pain, and bowel irregularities.
Qualifiers:
It is beneficial for people
- Having small and localized cancer which is wholly contained within a polyp
- Having a very early-stage cancer
Duration: It takes about 25 minutes to 1 hr.
Procedure details:
A polypectomy is carried out at the same time as a colonoscopy. A colonoscope (a long, thin, flexible tube with a camera and a light at the end) is inserted into the rectum to see colon segments.
A colonoscopy checks for any growths that could be indicative of cancer. If any polyps are discovered during colonoscopy, a polypectomy is performed.
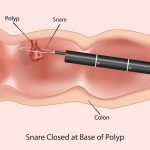
Polypectomy can be performed depending on the kind of polyps in the colon. It can be small, large, sessile, or pedunculated. Small polyps are removed (less than 5 millimeters in diameter) using biopsy forceps.
Polyps (up to 2 centimeters in diameter) are removed using a snare. In snare polypectomy, a thin wire is looped around the bottom of the polyp and uses heat to cut the growth off. The remaining tissue or stalk is cauterized.
Once a polyp has been removed, it is sent to a lab to test for malignancy. The results may take one week or longer.
Recovery
The recovery is quick. Minor side effects such as gassiness, bloating, and cramps usually resolve within 24 hours. With a more involved procedure, a full recovery can take up to two weeks.
Risks and complications
- Fever
- Infection
- Heavy bleeding
- Severe abdominal pain (Bellyache) or bloating in your abdomen
- Vomiting (Emesis)
- Irregular heartbeat
Post-operative care
- No driving for 24 hours.
- Avoid drinks and foods (tea, coffee, soda, spicy food, alcohol) that can irritate the digestive system
- No strenuous activity
Endoscopic mucosal resection (EMR)
Large polyps might be removed during colonoscopy using special tools in a procedure called an endoscopic mucosal resection. It is an outpatient procedure that removes tumors just beneath the gastrointestinal (GI) wall without surgery. Using an endoscope, the gastroenterologists can see inside the body with a high degree of detail. At the same time, growths are removed, such as upper GI or colon polyps that might otherwise require surgery.
Qualifiers
It is beneficial for people having
- Early staged colon cancer
- A tumor that has not yet reached more profound layers of the GI wall
- A tumor that is more significant than two cms
Duration
It takes around 1 -3 hours
Procedure details
During the procedure, an IV is inserted to deliver a sedative. A high-definition endoscope is placed through the mouth or anus, depending on the location of the tumor. The doctor observes the images on a screen. It helps avoid damage to surrounding tissue during the procedure. Sometimes suction is applied to the top of the tumor, further lifting it up and away from other tissue.
A thin wire rope is placed around the base of the tumor. An electrical current in the wire cuts the tumor from the body and seals the cut simultaneously. The tumor is retrieved by suction or a retrieval tool with the endoscope. The tissue is pulled through the endoscope.
Recovery
Since there is no incision, most patients return home the same day. Recovery is faster and with less pain than from open or laparoscopic surgery.
Risks and complications
Post-operative care
- Avoid driving for few days
- Do not make any important decisions
- Avoid operating any heavy machinery
- Avoid any strenuous activities
Minimally invasive surgery (Laparoscopic surgery)
Polyps that can’t be removed using colonoscopy may be removed with laparoscopic surgery. Laparoscopic surgery has short-term benefits while maintaining equivalent oncological outcomes.
Qualifiers
Ideal candidates are those having
- Early-stage cancer
- Less advanced cancer
- No prior major surgeries
- Fewer radiation treatments
- Lower Body Mass Index (BMI)
Duration
It takes around 30 – 60 minutes
Procedure
Laparoscopy is carried out under general anesthesia. The surgeon makes multiple minor incisions in the abdomen to insert the laparoscope (a little surgical tool and a tube to pump gas into the stomach) so that the surgeon can look around and operate. The gas is let out of the stomach after the procedure is completed. The incisions are closed using stitches, and a dressing is applied.
Recovery
Recovery may take around 1 – 2 weeks to 2 – 4 weeks.
Risks and complications
- Reaction to anesthesia
- Blood clots
- Infection
- Pneumonia
- Fistula formation (abnormal hole).
- Damage to surrounding organs (intestines, bladder, blood vessels)
- Development of adhesions/scar tissue
- Bowel obstruction
- Incisional hernia
Post-operative care
- No heavy lifting for 4 to 5 weeks after surgery
- Avoid straining to have a bowel movement
- Take medications as directed.
- Resume normal activities such as work (dependent on the type of work), light physical activity, driving, walking upstairs, and sexual activity when advised
- Shower instead of a bath. Avoid tub bathing.
- Advance your diet as instructed. Eat a low-residue diet for 3 weeks following surgery.
- Drink 8 to 10 glasses of water daily unless otherwise instructed
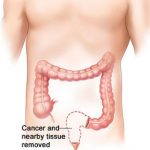
Partial colectomy
The surgeon may recommend partial colectomy if cancer has spread into or through the colon
It is a surgical process in which part or entire colon is removed. It is a commonly used treatment for colon cancer, although it may also be recommended for treating stomach cancer that has spread to the colon. Sometimes, a preventive colectomy is recommended if there is a high risk of developing colon cancer. Colectomies are helpful to treat large polyps and other conditions such as colitis and Crohn’s disease.
The different forms of bowel resection depend on the length of the colon (and sections) to be removed. These include:
Total colectomy (eliminating the whole colon)
Hemi-colectomy or Partial colectomy (removing half of the colon)
Left hemicolectomy (removing the left half of the transverse and the descending colon)
Right hemicolectomy (removing the right half of the transverse and the ascending colon)
Qualifiers
It is helpful for patients
- Having early-stage cancers
- Who require only a small section of the colon to be removed during colectomy
- Cancerous polyps or tissue growths in the colon
Duration
A hemicolectomy takes about two hours or longer, depending on any complications during the procedure.
Procedure
The cancerous part is removed along with a margin of normal tissue on either side of the cancer. The surgeon will make a few minor incisions in the abdominal area.
After making the incisions, the affected part of the colon is removed. Also, any part of the intestine connected to the part of the colon being removed is eliminated. The surgeon will remove lymph nodes and blood vessels that are related to the colon.

Once the affected part of the colon is removed, the rest of the colon is reconnected. This re-joining is known as anastomosis. If the surgeon can’t re-join the colon to another part of the digestive tract, they may join the colon to the abdominal skin. It is called a stoma, and you may need to wear a bag on your abdomen to store your waste after the surgery. Based on your surgery, this solution may be temporary or permanent.
Recovery
A hemicolectomy is major surgery. You may not be able to get back to normal activities for several weeks or more afterward.
Risks and complications
- Bleeding
- Blood clots
- Infection
- Fistula formation
- Development of adhesions/scar tissue.
- Bowel obstruction
- Incisional hernia
- Anastomotic leak
Post-operative care
- Avoid heavy lifting following surgery
- Avoid strenuous activity
- Take all medications as directed
- Resume your normal activities when advised
- Do not drive under the influence of medications.
- Take a shower instead of a bath
The prognosis of colon cancer
It depends on
Stage of cancer – Localized stage 0 cancers present with a better outcome than distant-stage three or four tumors. Early detection improves the prognosis and enhances life expectancy.
Grade of cancer – Higher the grade, more is the difference between normal and cancer-looking cells worse is the prognosis.
Lymph nodes involvement – Cancer metastasizes through the lymph. If more lymph nodes are involved, the prognosis might get worse.
Age – Prognosis is worse in elderly people.
Size and location of tumor – If the location or size of the tumor blocks the colon or creates a hole in the colon, it may affect the prognosis adversely.
General health condition – Better is the patient health likely they are to bear with cancer treatment and turn out cancer-free.
Carcinoembryonic antigen – With colon cancer, the blood CEA (protein molecule found in the blood) levels may increase, affecting a patient’s response to treatment.
Pre-operative evaluations prior to colon cancer surgery
- Do not eat or drink anything after midnight the night before surgery.
- Take medication as prescribed. Avoid any medicine containing aspirin for one week before the surgery.
- Do not smoke before surgery.
- Avoid wearing make-up, especially eye make-up, lotions, or powders.
- Do not wear nail polish. Your nails are monitored during surgery to identify oxygen and blood circulation.
Questions to ask your doctor
Why do I need colon surgery?
Are there any other treatment options?
What type of colon surgery procedure will I need?
How long will the surgery take? When can I go home?
What are the restrictions after the surgery?
What kind of assistance will be needed at home?
When can I resume my daily activities?
What medications are needed before and after the surgery?
How to take my usual medications?
How to manage post-surgery pain?
What kind of rehabilitation and physical therapy is needed?
When should I follow up with you?
How should I contact you?
Call your healthcare provider if you have
- Worsening or unrelieved pain
- Fever.
- Persistent vomiting, worsening abdominal pain or swelling.
- Signs of infection such as bleeding or drainage.
- Lack of bowel movement for 2 to 3 days.
- Any other concerns or questions